HOW DOES THAT WORK? - Cardiac Implantable Devices
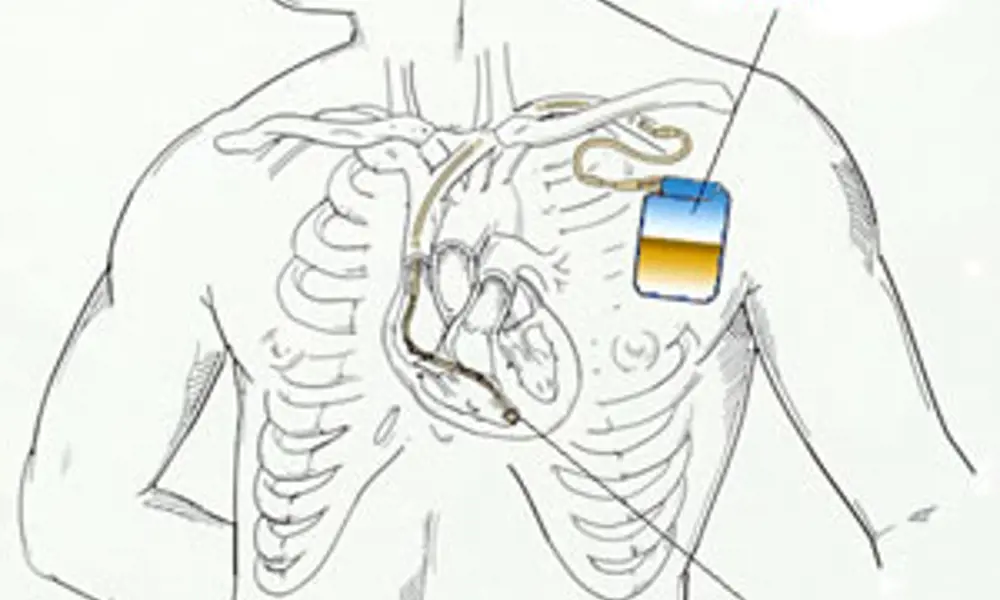
An automatic implantable cardioverter defibrillator (AICD) - Wikimedia Commons
Cardiac implantable devices have come a long way from the earliest pacemakers, and can now be used to treat – and diagnose – heart conditions beyond simple heart block (disruption of electrical pulses).
Developed in the 1950s, the earliest pacemaker devices were external, and used vacuum valve technology and mains power to ‘pace’ the heart with low voltage pulses. The development of the transistor in 1956, and the regulatory climate of the 1970s, paved the way for a booming industry producing small, battery-powered, implantable and safe devices.
These early pacemakers stimulated the heart without taking account of spontaneous cardiac activity, and could not change their pacing rate in accordance with a user’s physiological demands, for example, running. None of the parameters of the pacemaker could be changed. To solve this problem, modern implantable cardiac devices now contain microprocessors and dedicated integrated circuits which can be programmedin situ with a hand-held controller. They also contain sensors, and provide diagnostic information to the controller. Some devices use their sensing functions to detect, for example, tachycardia (an unnatural fast heart rate, over 100 bpm) and life-threatening ventricular fibrillations (where the heart stops pumping). The devices can treat these conditions with complex pacing routines and internal electric shocks to re-start pumping, in a similar process to the use of defibrillation paddles.
Engineers are now developing software algorithms to detect whether a fast heart rhythm is truly dangerous, or the result of patient activity, as well as trying to improve the size, reliability, and efficiency of these cardiac devices.
Keep up-to-date with Ingenia for free
SubscribeOther content from Ingenia
Quick read

- Environment & sustainability
- Opinion
A young engineer’s perspective on the good, the bad and the ugly of COP27

- Environment & sustainability
- Issue 95
How do we pay for net zero technologies?
Quick read

- Transport
- Mechanical
- How I got here
Electrifying trains and STEMAZING outreach

- Civil & structural
- Environment & sustainability
- Issue 95