Mobile health technology
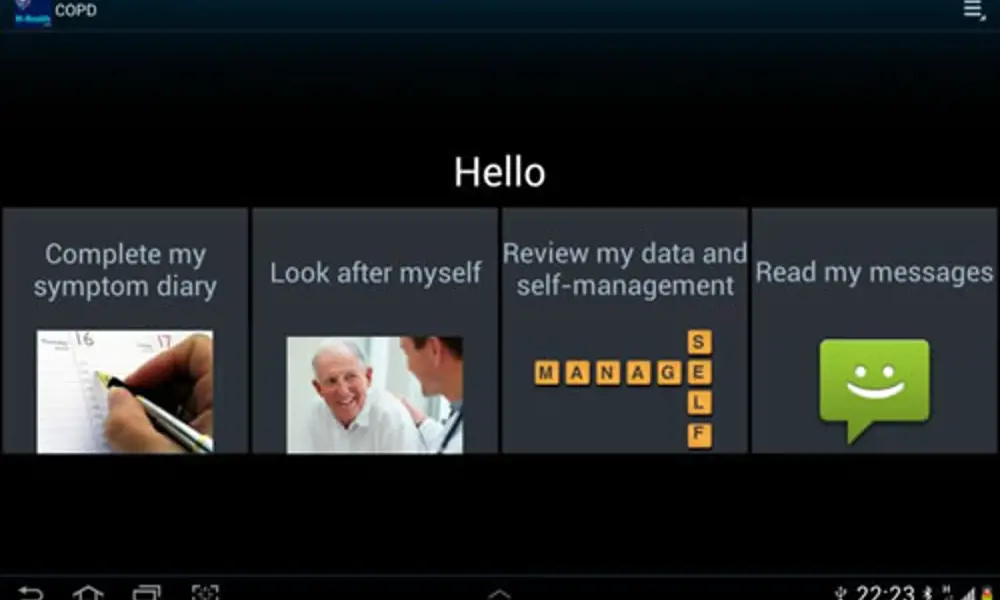
Screenshot from m-health app for self-management of COPD running on an Android tablet (Samsung Galaxy Tab)
The growth of sensor-enabled phones and tablets, coupled with Bluetooth technology and a robust mobile network infrastructure, is enabling the spread of mobile health technologies for patient self-monitoring. These systems can provide instant feedback and prioritise care needs, while reducing the demand on NHS resources. Professor Lionel Tarassenko CBE FREng FMedSci explains how engineers are working with clinicians to develop monitoring systems that keep patients healthier by helping them manage their conditions better.
The NHS is spending increasing amounts of its budget looking after patients with chronic diseases. This problem affects healthcare providers worldwide, as people are living longer with chronic conditions such as diabetes, heart disease or respiratory disease. Within the NHS, patients with these conditions account for half of all GP appointments, two thirds of outpatient appointments and three quarters of inpatient bed days.
Improved self-management by patients, together with regular support from healthcare professionals, can reduce healthcare spending on chronic disease. Patients who are able to self-manage are more likely to have fewer unplanned hospital admissions or emergency visits to their GP and will take fewer days off work.
The challenge is to create solutions which can both support self-management and be fully integrated within the healthcare delivery process, without adding significantly to the workload of overstretched clinicians.
MOBILE TECHNOLOGY
‘Telehealth’ has been defined by the Department of Health as a service that ‘uses equipment to monitor people’s health in their own home… [monitoring] vital signs such as blood pressure, blood oxygen levels or weight’. The data are transmitted via broadband or a dial-up telephone line to a monitoring centre or health care professional. Mobile health, or m-health, is a development of telehealth which allows patients to use mobile communications technology rather than fixed, dedicated devices in the home. The development of m-health started a decade ago when General Packet Radio Service (GPRS) and 3G networks brought increased data capability to European mobile telecommunications. This made it possible to transfer data to and from a remote web server in real time using just a mobile phone with a SIM card. This has encouraged the development of software applications to turn the mobile phone into a tool for self-management. From the patients’ point of view, the technology allows real-time feedback, through trend plots and colour displays, enabling them to adjust medication dosage within the parameters of their treatment plans.
The recent convergence between computing and communications, seen in computer tablets such as the iPad and the Samsung Galaxy Tab, has further increased the potential impact of m-health on chronic disease management. A large proportion of the target population consists of elderly people. Developing a user interface which is intuitive and easy to use by patients with no experience of computer usage and who also may be suffering from significant hand tremor has been solved by replacing the keyboard with large icons on tablets with large touch-sensitive screens.

m-health app for gestational diabetes. The graphical displays on an Android phone show pre- and post-meal readings
ACTIVE MONITORING
The concept of providing equipment for patients to self-manage is not new. Asthma patients have been able to take peak air flow readings (measuring a person’s ability to breathe out) at home for 50 years. Blood glucose and blood pressure are two other examples of vital signs that can easily be monitored by a patient at home. Data can now be transmitted automatically from medical devices (such as glucometers) to mobile phones using Bluetooth technology. The self-monitoring and symptom diary functions are integrated in a software application on a phone or tablet, which provides personalised feedback. The use of m-health apps can deliver improved patient outcomes for short-term, focused interventions such as insulin initiation for people with type 2 diabetes.
Patients with type 1 diabetes have been self-managing their condition by monitoring blood sugar levels since the introduction of electronic glucometers more than 40 years ago. This enables them to inject the right amount of insulin to prevent blood glucose concentrations getting too high (thereby minimising the long-term risk of stroke, kidney disease or blindness) but also to avoid hypoglycaemic events (such as dizziness or even coma) which may occur when blood glucose levels suddenly drop.
Keeping to this routine can be onerous, especially for young people with the condition. Research in Oxford has shown that providing patients with an electronic glucometer linked to a mobile phone via Bluetooth can help self-management. In one of the first trials of m-health, young adults with type 1 diabetes were provided with a Bluetooth-enabled glucometer, a mobile phone, and an electronic patient diary app on the phone. The participants in the intervention group were also given extra feedback in terms of colour-coded screens which summarised their glucose control over the past 48 hours and previous month. Those patients also had additional support by phone from a diabetes nurse who had web access to the self-monitoring data. The results after nine months showed that diabetes control improved in both groups, but those in the intervention group had an even greater improvement in their blood glucose control – and hence a reduced risk of serious long-term complications.
The m-health technology has also been tested in patients with type 2 diabetes who needed to start insulin injections. Within this group, the mobile phones had pre-loaded software which provided guidance on selecting the right dose of insulin. Again, patients were found to have improved glucose control at the end of the trial. The technology is now being deployed on Android phones to support women with gestational diabetes during the last three months of their pregnancies.
TECHNOLOGY AND SECRUITY
Technology is important, but the development of long-term monitoring strategies requires an understanding not only of the patients’ physiology but also of their psychology. The need for patients with chronic diseases to self-monitor and self-manage is a daily reminder that they have a long-term condition.
With elderly patients who are mostly confined to their homes, the provision of a modern multi-purpose computer tablet removes some of the stigma sometimes associated with dedicated telehealth equipment. The large screens also allow patients access to multimedia options such as videos to support self-management; for example, with demonstrations of inhaler techniques – see COPD.
An important component of any m-health system is the secure, remote server which stores the patient data transmitted by the mobile phone or tablet. Algorithms running on this server can be used to prioritise patients for healthcare professionals to call, if needed.
Patient data are typically held on an NHS server which requires all access to be via encrypted connections (SSL). To increase security, a patient’s website locks out after a small number of incorrect login attempts. The m-health software is only installed on tablets configured for chronic disease management. The tablet software also includes a ‘remote wipe’ feature which can be used to erase patient data if a tablet is lost or stolen.
TECHNOLOGY SUPPORTS
Engineering has a substantial underpinning role to play in improving the care and support of patients through m-health. Successful technological innovation in chronic disease management has required engineers to develop not only an understanding of the patients’ physiology but also of their psychology. For this to happen, there has been a need to work in multidisciplinary teams, which include patients, nurses, GPs and consultants, when designing m-health apps which encourage high levels of patient compliance with self-monitoring.
The combination of increased compliance, personalised feedback to support self-management and the use of machine learning algorithms to track patient-specific changes in symptoms and vital signs is likely to lead to increasingly large-scale adoptions of m-health.
Keep up-to-date with Ingenia for free
SubscribeOther content from Ingenia
Quick read

- Environment & sustainability
- Opinion
A young engineer’s perspective on the good, the bad and the ugly of COP27

- Environment & sustainability
- Issue 95
How do we pay for net zero technologies?
Quick read

- Transport
- Mechanical
- How I got here
Electrifying trains and STEMAZING outreach

- Civil & structural
- Environment & sustainability
- Issue 95