
The affordable diagnostic tool saving sight in low-income countries

A doctor uses the Arclight in Rwanda © Mrs Claire Morton, consultant ophthalmologist
The Arclight is an affordable, solar-powered ophthalmoscope, a diagnostic tool that is used by health workers to view the interior of the eye and detect early signs of blindness. The device was developed over five years by researchers at the University of St Andrews. Its compact size and small price tag, coupled with its ability to harness solar power, mean that it can be useful to clinicians working in low-income and remote locations.
Ophthalmoscopes are essential for diagnosing nearly all eye abnormalities, enabling skilled users to see the front and back of the eye and revealing conditions such as cataract, glaucoma and trachoma, which can all cause blindness. The instruments can be expensive, so availability can sometimes be limited. Around 220 million people around the world are visually impaired or blind, 80% of whose blindness would have been avoidable if treated, according to the World Health Organization.
Around 220 million people around the world are visually impaired or blind, 80% of whose blindness would have been avoidable if treated
Optometrist William J Williams, who is Director of Arclight Medical and an Honorary Research Fellow at the University of St Andrews, set out 10 years ago to produce a portable, intuitive and affordable diagnostic tool. He came up with the idea for the Arclight by stripping unnecessary features from a traditional direct ophthalmoscope.
Supported by a team at the university and awarded £100,000 from The Fred Hollows Foundation, his breakthrough was swapping the traditional filament bulb, which can be difficult to replace in remote communities, for a cool, low-energy LED. The design eliminates the need for the mirror and optics inside conventional ophthalmoscopes, replacing them with an LED facing the patient. This is closely aligned with a sight-hole that produces near coaxial light paths to give the user a dust-free view of the eye’s interior. Clinicians can also use a slider on the device to focus and adjust its lighting level.
The current instrument includes a slot-in PCB (printed circuit board) module that has a micro USB port, and lenses so that it can be charged if needed, while an integrated solar panel means that it can be used as an ‘off-grid’ diagnostic tool. When a small plastic tube is added to the magnification loupe, the Arclight can be transformed into an octoscope to diagnose hearing conditions.
When a small plastic tube is added to the magnification loupe, the Arclight can be transformed into an octoscope to diagnose hearing conditions
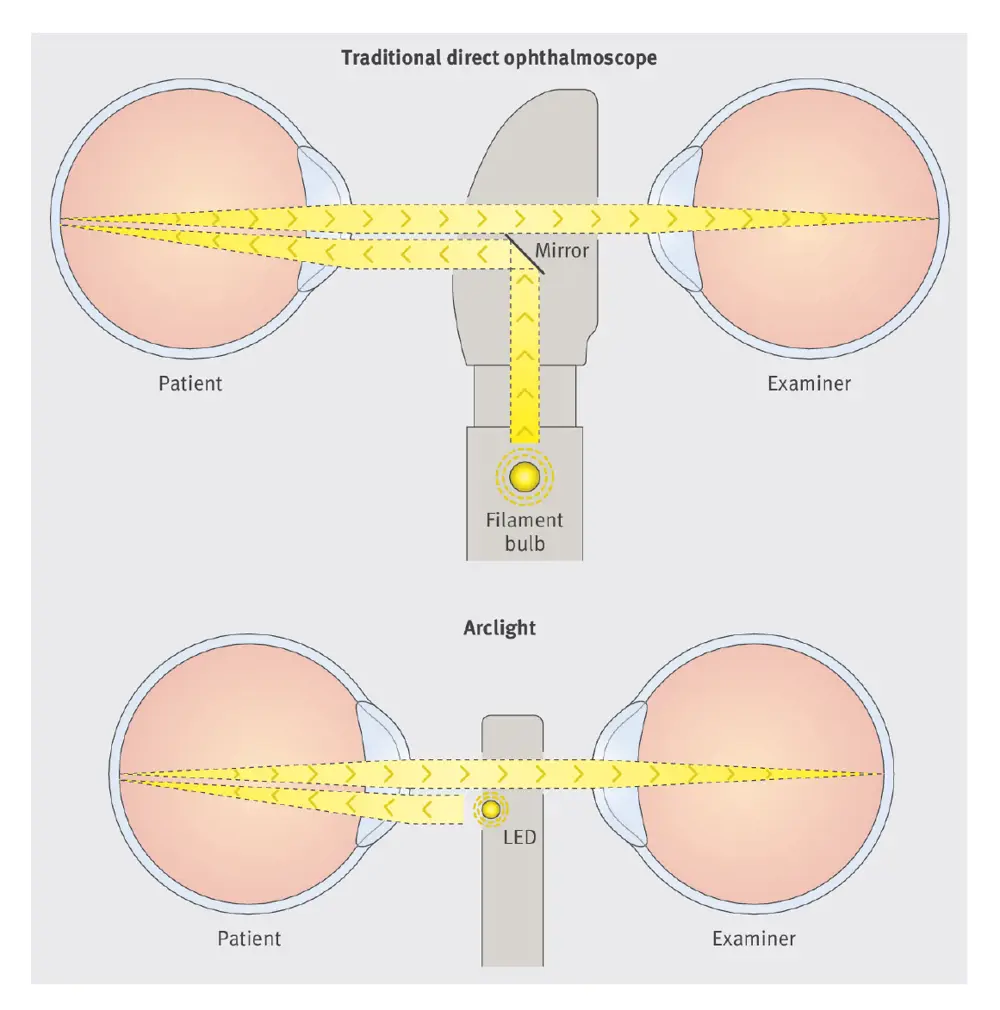
A diagram shows how the Arclight’s LED differs from the traditional bulb and mirror
A study led by the International Centre for Eye Health in London revealed that the Arclight is at least as good as traditional ophthalmoscopes, and is better in some areas, such as size and ease of use. It has been listed as one of the International Agency for the Prevention of Blindness’ recommended devices for use in low- and middle-income environments. More than 10,000 Arclights have been distributed in over 50 countries, including Malawi, Ghana, Ethiopia, Rwanda, Fiji, Indonesia and the Solomon Islands.
While this version of the Arclight is already changing lives, version three will include internal memory loaded with teaching resources for clinicians in remote areas. The teaching tools can be viewed by attaching a mobile phone without the need for an internet connection.
The company hopes that Arclight will become more widely available in communities where it is needed. By selling the devices to doctors in richer countries at a profit, a social enterprise run through the University of St Andrew’s global health team have helped to fund the roll-out of cost-price devices in poorer communities.
For further information, visit arclightscope.com
***
This article has been adapted from "Saving sight in developing countries", which originally appeared in the print edition of Ingenia 72 (September 2017)
Keep up-to-date with Ingenia for free
SubscribeRelated content
Health & medical

Kidney dialysis
Small haemodialysis machines have been developed that will allow more people to treat themselves at home. The SC+ system that has been developed is lighter, smaller and easier to use than existing machines.

Engineering polymath wins major award
The 2015 Queen Elizabeth Prize for Engineering has been awarded to the ground-breaking chemical engineer Dr Robert Langer FREng for his revolutionary advances and leadership in engineering at the interface between chemistry and medicine.
Blast mitigation and injury treatment
The Royal British Legion Centre for Blast Injury Studies is a world-renowned research facility based at Imperial College London. Its director, Professor Anthony Bull FREng, explains how a multidisciplinary team is helping protect, treat and rehabilitate people who are exposed to explosive forces.
Targeting cancers with magnetism
Cambridge-based Endomag has helped treat more than 6,000 breast cancer patients across 20 countries. The MacRobert finalist uses magnetic fields to power diagnostic and therapeutic devices. Find about the challenges that surround the development and acceptance of medical innovations.
Other content from Ingenia
Quick read

- Environment & sustainability
- Opinion
A young engineer’s perspective on the good, the bad and the ugly of COP27

- Environment & sustainability
- Issue 95
How do we pay for net zero technologies?
Quick read

- Transport
- Mechanical
- How I got here
Electrifying trains and STEMAZING outreach

- Civil & structural
- Environment & sustainability
- Issue 95