
Keeping transplant livers alive
Until recently, doctors who had identified and removed a potentially suitable liver for organ donation would cool it to 40°C, place it in an ice box, and transport it as quickly as possible to one of the surgical centres where it could be used. This might take several hours – during which time it was hoped that the liver would lose as little as possible of its functional capacity.
Like surgeons before him, Peter Friend, Professor of Transplantation at the University of Oxford, reasoned that the chances of preserving a liver during its time outside the body might be enhanced if, instead of cooling the organ, it could be kept at body temperature in conditions as similar as possible to those it normally experienced. As well as keeping the temperature constant, a continuous blood supply could bring the liver oxygen and other nutrients.
This ‘normothermic’ strategy had in fact been tried a number of times in the past, but without success. By going back to basics, and learning more of the biology of the liver, Friend – working closely with colleague Professor Constantin Coussios FREng of the Oxford Institute of Biomedical Engineering – devised a successful method of achieving this goal. Coussios and Friend set up a company called OrganOx to develop a practicable machine for preserving isolated livers under physiological conditions. The OrganOx metra® is now on the market.
Liver transplantation
🩺 When are liver transplants necessary and why do the number of livers available not meet the available need
A liver transplant becomes necessary when the recipient’s own organ is diseased or damaged beyond repair. The main causes of severe liver damage include cirrhosis, hepatitis, various metabolic conditions and paracetamol poisoning.
In the UK, more than a thousand livers are transplanted each year. But this number does not meet the full extent of the need. The average waiting time for a liver transplant in the UK is more than 130 days for adults and more than 70 for children. Not surprisingly, some patients die while on the waiting list.
Many potential donor organs cannot be used because their condition is sub-optimal. Such livers do not tolerate conventional cold storage and, until now, there has been no reliable way to assess the viability of an organ preoperatively.

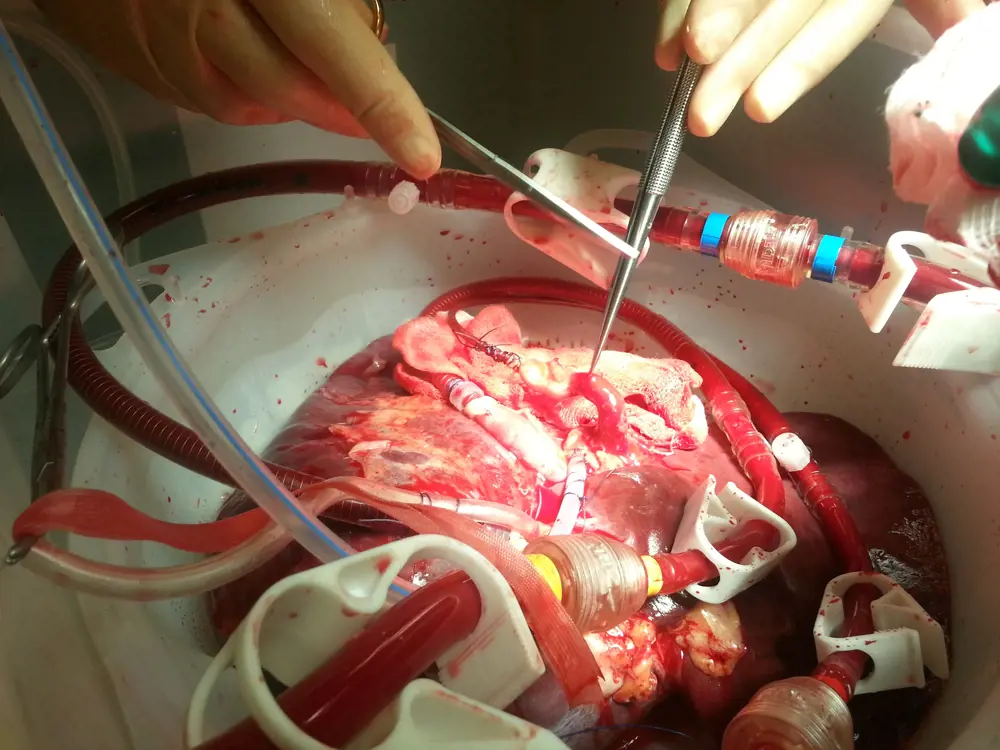
Preparing the OrganOx-preserved liver for connection © OrganOx
Replicating complex biology with over 40,000 components
In principle, the metra simply aims to replicate what goes on in the body – though ‘simply’ is a monumental understatement. A schematic flow chart of the machine’s ‘plumbing’ – its various components and the tubing that carries blood between them – reveals little of its complexity. Running the metra requires three units of blood, a little over 1.5 litres. Playing the role of the heart is a pump that initially pushes the blood through an oxygenator. The liver, unlike most organs in body, has two blood supplies, the hepatic artery and the portal vein. The metra mimics this arrangement. Some of the oxygenated blood is channelled directly to the isolated liver though a tube that enters the stump of the hepatic artery. The rest is pumped into a reservoir where nutrients, including insulin and heparin, to prevent clotting, are added.
Only then is this portion of the blood also channelled to the liver – in this case through the stump of the portal vein. Blood from both sources exits the liver via another vessel, the inferior vena cava, passes through a blood gas analyser, and re-enters the pump.
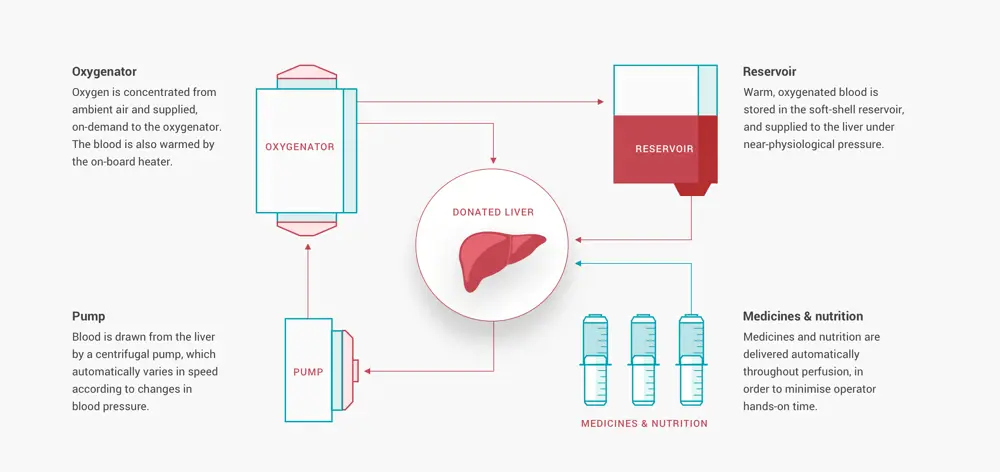
A flow schematic showing how the metra achieves machine perfusion for liver transplantation © OrganOx
In engineering terms, you may think, a fairly straightforward set up. Coussios knows otherwise, remarking that “biology really teaches engineers a lesson in humility”. You get a hint of this on learning that each metra comprises a staggering 40,000 components.
Previous failures of mimicking natural liver physiology
One reason why previous attempts to mimic the natural perfusion of isolated livers have failed is that these organs, even when detached from the body’s nervous system, retain the capacity to vary their resistance to blood flow going through them according to their need for oxygen or nutrients. These changes in resistance – and the consequential changes in the organs’ demand for blood – can be rapid. To cope adequately with such fluctuations in an artificial system proved to be a thorny problem.
Most researchers have tried to maintain physiological arterial pressure at the inlet to the organ by modulating the flow rate of the pump, thereby artificially setting the flow rate through the organ. But this, while relatively straightforward to achieve, is not how the body itself operates. The metra is designed not to maintain a constant flow of blood, but a constant pressure difference across the organ, enabling the organ to ‘choose’ its own blood supply. This well-known biological phenomenon is termed autoregulation. Achieving it was complicated by the liver’s exceptional plumbing: one outflow of blood, but two inflows. Imitating the natural physiology of the liver proved to be an engineering challenge that took years to overcome.
A liver being perfused on the metra © OrganOx
Control loops relying on sensors in a conventional engineering feedback system find it difficult, if not impossible to match the speed of natural biological control systems. In the first one to four hours following removal of a donated liver, changes within it are particularly rapid, and any physiologically abnormal perfusion can cause severe damage to the organ’s vasculature.
One way that Friend and Coussios minimised the problem was to choose components for their system that had a degree of autoregulation. An example is the type of pump that propels the blood around the metra and through the liver. In a roller pump of the kind used in most cardiopulmonary medical devices, the flow rate of the blood is determined by the roller’s speed of rotation. The metra uses a centrifugal pump in which the outflow is determined both by the rotational speed of the pump and by the downstream resistance. So if vessels in the liver undergo constriction, the outflow of the pump is instantly reduced even before its rotational speed has decreased. The organ is, in effect, controlling its own blood supply.
Imitating the natural physiology of the liver proved to be an engineering challenge that took years to overcome
This, however, throws up another problem. Any change in the resistance of the organ that requires a change in pump speed will precipitate a need to alter the settings of the other controls in the system, in particular the valves that regulate the flow and volume of blood passing through the liver. In fact, there are no fewer than seven independent controllers within the metra dealing not only with pressures and flows, as measured by flow sensors located at critical points, but with several other variables such as temperature, blood gas levels and nutrition. The needs of the isolated liver with respect to each of these variables were originally unknown; they had to be established through experiments before engineering to replicate them could begin.
Designing a strategy for the machine’s controllers was perhaps the greatest challenge of the whole project. As Coussios comments, working with a nonlinear system characterised by multiple inputs and outputs in which a change in one affects all the others is, to say the least, demanding.
More hurdles overcome
Also problematic, though for different reasons, was the supply of gas required by the metra’s oxygenation unit. Standard gas cylinders are too heavy and cumbersome to create a portable machine that can support an organ for 24 hours. The metra utilises oxygen concentration technology in a novel device that produces the gas in the required amount from the atmosphere, only when it’s needed. The oxygenator is also responsible for warming the blood to 37°C.
The body’s vascular system has evolved to do minimum damage to the red blood cells swept along within it. These cells are susceptible to shear stress of the kind often created by artificial devices. To overcome this it was necessary to measure and then optimise the design of every bend and twist in the fluid path. It might be imagined that the greatest source of shear stress would be the pump. In fact, it turned out that the most damage was done by vortices that formed in the blood as it passed through the valves. These had to be specially redesigned to minimise the emergence of such vortices.
The system’s blood reservoir takes the form of a soft flexible bag. Nutrients, such as heparin are introduced into the bag in predetermined quantities at a pre-set rate by means of a set of screw-driven syringes. From the reservoir, the blood flows into the liver via the second of its supply vessels, the portal vein. Although complicated in design and actions, the metra is surprisingly simple to use, and carries only ‘play’, ‘stop’ and ‘eject’ buttons: one of the reasons that it took so long to perfect. The machine is, as Coussios rather wickedly describes it, “virtually doctor proof”.

The metra can be loaded onto vehicles used by transplant teams. The protective hard covers for transport leave a space for the graphical user interface screen and the liver bowl to remain visible © OrganOx
A working liver and direct evidence of functionality
The donor liver itself is supported on a silicone rubber sling inside an enclosed box. This arrangement allows any fluid secreted by the organ to be collected and returned to the reservoir. The cut ends of the organ’s inflow and outflow vessels are fitted with cannulae designed to marry easily with the tubes of the machine.
A blood gas analyser takes continuous measurements of the oxygen and carbon dioxide levels and pH of the blood as it makes its return journey to the pump. These measurements, made in real time, are used by the machine’s internal controller to set the oxygen and air supply to the oxygenator.
Working livers secrete bile. Although this is ultimately discarded, the metra collects and measures the volume of bile produced: a useful guide to the functional state of the organ. Alongside all the other parameters measured, it provides what Coussios describes as an opportunity for the surgeon to ‘test drive’ the liver before reaching a final decision about its suitability for transplantation. With conventional cold preservation, the surgeon making this decision has little to go on other than the medical history of the donor and the overall appearance of the organ. Doctors using the metra have direct evidence of the organ’s functional condition. Data on its viability can, if required, be monitored remotely.
The metra is nothing if not robust. It weighs some 80 kilograms, the consequence of a rigid wheeled base which, together with its batteries, allows it to be moved around the hospital and transported by road. It can even withstand lateral accelerations of several times gravity and can therefore be moved by an aircraft should it need to be. In a larger country such as the US, this option can be essential. Using cold storage, donor organs have to be implanted within eight hours, or 12 at the most. With normothermic preservation this time can be stretched to at least 24 hours and, if combined with periods of cold storage, to 36 hours or more.
Real-world performance with a major impact on organ utilisation
The real-world performance of the metra has found support in a clutch of clinical trials. One of the most significant was published last year in Nature and involved 220 subjects at seven sites in Europe. The trial was set up to compare the transplantation of donor livers allotted at random to conventional cold storage or to normothermic preservation using the metra. The study demonstrated that, even though 50% fewer organs were discarded in the normothermic arm and these organs were preserved on average for 50% longer, survival outcomes were not compromised and post-transplant liver injury was reduced by 50% in the recipient. As the authors of the study commented, “If translated to clinical practice, these results would have a major impact on organ utilisation, liver transplant outcomes and waiting list mortality.”
The metra received its CE mark in 2016, and was granted approval by NICE (the National Institute for Clinical and Health Excellence) in 2019. It is now used in every transplantation centre in the UK, and in almost every country in Europe. An application for US approval is currently in progress. More than 550 livers have now been successfully preserved and transplanted in 11 countries. OrganOx is already well advanced on a machine for the normothermic preservation of donor kidneys, with a clinical trial due to commence in early 2020. The innovation made the shortlist for the Royal Academy of Engineering’s MacRobert Award in 2019.
However, probably one of the most important outcomes is the fact that liver transplantation can now become a planned rather than an emergency procedure
OrganOx is not alone in the warm preservation field; two other companies are active, but less far advanced. One measure of OrganOx’s success is that all its original investors are still backing it, and it is still the only technology to have successfully completed a randomised clinical trial providing firm evidence of efficacy.
However, probably one of the most important outcomes is the fact that liver transplantation can now become a planned rather than an emergency procedure. The operation can now take place at a time that is best for the clinical team, patient and hospital. Medical journals have noted that this has several significant effects including reduced costs and more successful outcomes for the patient.
***
This article has been adapted from "Keeping transplant livers alive", which originally appeared in the print edition of Ingenia 81 (December 2019).
Contributors
Geoff Watts
Author
Peter Friend is Professor of Transplantation at the University of Oxford and Director of the Oxford Transplant Centre. He is a founder of OrganOx and Chief Medical Officer, with primary responsibility for the pre-clinical and clinical trials of OrganOx’s patented normothermic organ perfusion technology. Peter’s research interests lie primarily in novel applications of normothermic organ perfusion
Constantin Coussios FREng is Professor of Biomedical Engineering at the University of Oxford and Director of the Oxford Institute of Biomedical Engineering. He is a founder of OrganOx and Chief Technology Officer, and leads the company’s research and development activities. Professor Coussios received the 2017 Royal Academy of Engineering Silver Medal and was appointed as a Fellow of the Royal Academy of Engineering in 2019.
Keep up-to-date with Ingenia for free
SubscribeRelated content
Health & medical
A gamechanger in retinal scanning
2006 MacRobert Award winner Optos rapidly became a leading medical technology company and its scanners have taken millions of retinal images worldwide. There is even a display at the Science Museum featuring the Optos development. Alastair Atkinson, of the award-winning team, describes the personal tragedy that was the trigger for the creation of Optos.

Kidney dialysis
Small haemodialysis machines have been developed that will allow more people to treat themselves at home. The SC+ system that has been developed is lighter, smaller and easier to use than existing machines.

Engineering polymath wins major award
The 2015 Queen Elizabeth Prize for Engineering has been awarded to the ground-breaking chemical engineer Dr Robert Langer FREng for his revolutionary advances and leadership in engineering at the interface between chemistry and medicine.
Blast mitigation and injury treatment
The Royal British Legion Centre for Blast Injury Studies is a world-renowned research facility based at Imperial College London. Its director, Professor Anthony Bull FREng, explains how a multidisciplinary team is helping protect, treat and rehabilitate people who are exposed to explosive forces.
Other content from Ingenia
Quick read

- Environment & sustainability
- Opinion
A young engineer’s perspective on the good, the bad and the ugly of COP27

- Environment & sustainability
- Issue 95
How do we pay for net zero technologies?
Quick read

- Transport
- Mechanical
- How I got here
Electrifying trains and STEMAZING outreach

- Civil & structural
- Environment & sustainability
- Issue 95