Wastewater epidemiology
Viruses are some of the simplest biological structures on earth. They are not ‘alive’ and cannot replicate outside of their host. How do you track infectious disease outbreaks at the scale of countries or continents? Lack of available testing in most countries, either in the form of quantitative methods or medical tests, prevent a public health response to the ‘rapidly rising tide’ of cases that occurs in easily transmitted infectious diseases. This includes the current pandemic virus – SARS-CoV-2. Testing is invasive, difficult to perform and requires repeat testing of individuals who are susceptible to the disease, so other approaches are needed.
It is common for people infected with viruses to release them in poo and wee. Therefore, one popular approach to monitor outbreaks is wastewater-based surveillance (WBS). Before COVID-19, it was used for monitoring polio and drug use. The value of WBS is that decision-makers can estimate the amounts of disease circulating in the population with only a few samples. In total, tens of thousands of researchers in over 50 countries are undertaking WBS for SARS-CoV-2. Alongside the vaccination roll-out, it is one of the biggest mobilisations of scientists since the Second World War for a single vision.
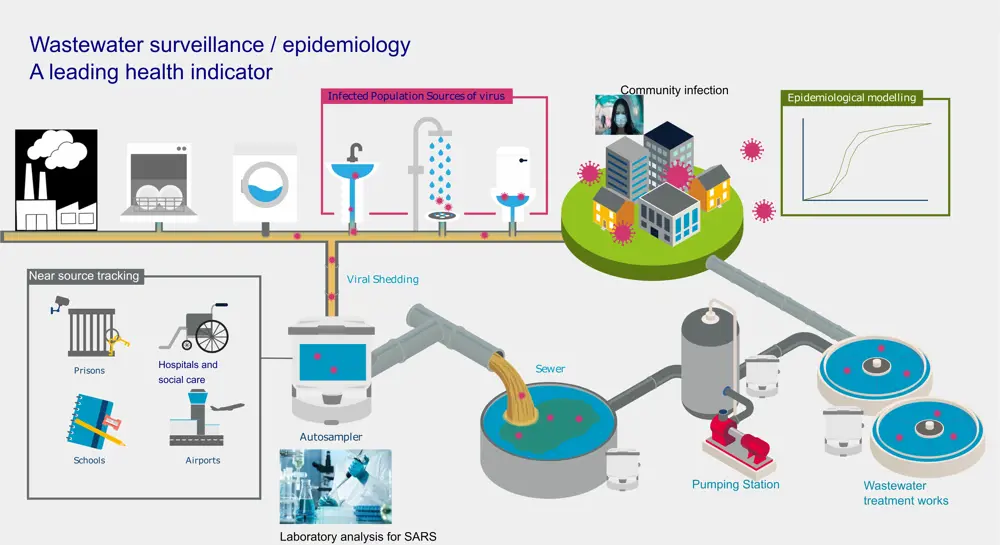
The process for tracking the spread of viruses through wastewater
Grab samples or a dedicated automatic sampling device are set up at various points in the sewage/wastewater infrastructure. This includes discharge points from large buildings like schools and hospitals, sewage pipes, and at water recycling centres (sewage works). Some countries like China have also started monitoring toilets and the swabs and poo obtained directly from individuals. Thankfully, the UK is not sampling ‘at source’ yet… Collecting wastewater with respect to COVID-19 is safe; the World Health Organization suggested in 2020 that wastewater does not represent a friendly environment for this virus and so is unlikely to infect people.
However, many challenges remain in the collection, analysis and interpretation of this data. On the wastewater side, municipal sewage is often changed by industry inputs and rainfall from roads and buildings. These inputs to the sewage system do not contain the ‘signal’, which is the virus fragments (RNA), but contain lots of dilution in the best case or ‘noise’ in the worst case. On the medical side, one aspect we do not understand well with SARS-CoV-2 is faecal shedding. This is the number of viruses each infected individual will shed in the faeces (in this case) or nose and throat for mass testing. At present we don’t fully understand how long people will shed the virus and how long it will be detectable in wastewater. Another question is whether children or vaccinated individuals shed viruses to the same extent. Or how poo shedding changes in people infected with different variants (mutant strains of the virus). These factors are important to interpretation of the data for wastewater surveillance. One further challenge is how to monitor in ‘low-prevalence’ scenarios – this is where the number of infected individuals drops due to lockdowns, vaccination or natural immunity. Wastewater surveillance has been credited as one of the big success stories of the pandemic, helping governments respond in a rapid way without infringing the ethics and data protection rights of individuals. A major challenge is communicating the results of these surveys to the public in an appropriate way.
Keep up-to-date with Ingenia for free
SubscribeRelated content
Chemical

Q&A: Olivia Sweeney
Olivia Sweeney sources aroma chemicals to create fragrances at cosmetics company Lush. She is working on finding new, more sustainable sources of fragrance ingredients, with an interest in the research and development of chemical production from waste streams.

Biofuels’ journey to the mainstream
Liquid biofuels today make up about 8% of road and non-road fuel supplies in the UK. The government plans to reach nearly 10% by 2020 in order to reduce CO₂ emissions. It has also laid out targets to incentivise innovation and the production of ‘development fuels’.

Compostable plastics
Compostable plastics can be turned – alongside food and other organic waste – into compost. But how environmentally friendly are they really?

Q&A: Michelle Watiki
From placements at Xerox and Rolls Royce, to becoming a board member for the Association for Black and Ethnic Minority Engineers, chemical engineering graduate Michelle Watiki hopes to apply her knowledge to sustainability and net zero, as well as helping future engineering students.
Other content from Ingenia
Quick read

- Environment & sustainability
- Opinion
A young engineer’s perspective on the good, the bad and the ugly of COP27

- Environment & sustainability
- Issue 95
How do we pay for net zero technologies?
Quick read

- Transport
- Mechanical
- How I got here
Electrifying trains and STEMAZING outreach

- Civil & structural
- Environment & sustainability
- Issue 95