
Developing the first integrated prosthetic leg
Much as he enjoys winning awards for engineering and personal honours, ask Professor Sir Saeed Zahedi OBE RDI FREng to recall his most satisfying achievement, and he cites assembling and managing the team that developed the world’s first integrated prosthetic leg. Still an unmatched example of biomedical engineering, the Linx was the first microprocessor-controlled lower limb prosthetic where the foot and knee continuously ‘talk’ to each other. In this way, the Linx can create a more natural leg movement. With its combination of new materials, microprocessor controls and understanding of how people walk, Linx won the 2016 MacRobert Award. It has since gone on to restore mobility to more than 500 individuals a year.
This revolution in prosthetics started when Sir Saeed assembled a team of mechanical engineers, electronic engineers, and physiotherapists, among others, to work together on Linx at Blatchford Group. “Watching 30 people is almost like conducting an orchestra,” he says. “You’re not even telling them what to do, you are just pointing towards what they need to do.”
Biomedical engineering was hardly a mainstream subject when Sir Saeed decided to improve his qualifications so that he could help people who had lost limbs in accidents and conflicts. Looking for somewhere to add a master’s degree to his background in mechanical engineering, he had the choice of just two universities in the UK and there were few students keen to work in the area: “In my year, there were nine students and 16 lecturers.”

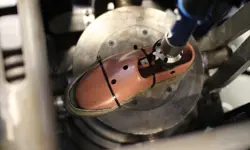
The 2016 MacRobert Award-winning Linx limb system, developed by Blatchford, is the first ever prosthetic limb with integrated robotic control of the knee and foot, in which the sensors work together so that users can walk, balance and be supported on all types of terrain © Blatchford
Learning engineering
Sir Saeed ascribes his own introduction to engineering partly to a need to find a subject to study where language would not be a hindrance. Born in Iran, his first language was Farsi. When his family decided that he should continue his education in the UK, he picked A-level subjects with mathematics at their core. He considered medicine, but the advice was that it required, as he puts it now, “a greater command of English”.
Like many engineers, Sir Saeed knew little about engineering when he was considering his future career. He did have an early interest in how things worked and his father bought the local equivalent of New Scientist. “Reading it was a natural interest in engineering, without knowing what engineering really was,” he says. When it came to looking for a career, he started by eliminating the things that he did not want to do. “I knew that I wasn’t going to be a businessman, or a lawyer, or an economist, or go into literature.” Mechanical engineering won the competition. Looking back, he says, as a youngster he had been interested in recycling and biomedicine, attracted by the human social benefits they offered.
After A levels, he attended the Polytechnic of Central London (now the University of Westminster) to study mechanical engineering. Polytechnics, with their roots in engineering and focus on vocational studies, gave graduates industry-friendly courses and professional qualifications. The polytechnic also gave students access to advanced manufacturing systems, through the college’s links with companies such as Short Brothers, where Sir Saeed spent time learning about computer numerical control (CNC) programming and making parts for aircraft.
Sir Saeed’s degree offered biomedical engineering as a final-year option, so while he investigated the use of CNC, he also did work with Northwood Park Hospital using force platforms, which are instruments that measure the ground reaction forces generated by a body standing on or moving across them, to quantify balance, gait and other parameters of biomechanics.
“When I finished my degree, I had a choice of going for a job in Short Brothers or doing a master’s in biomedical engineering at the University of Strathclyde”, one of the two places in the UK that ran courses in biomedical engineering.
Sir Saeed recalls checking a government website and seeing that it touted biomedical engineering as the “number one topic for promoting careers in engineering”
At Strathclyde, Sir Saaed’s ambition was to apply CNC technology to custom-build hip replacements. However, his supervisor and mentor, Professor John Paul FREng FRSE, suggested that the health service and technology was not ready at the time and guided him into work on lower-limb prosthetics. In part this was down to the state of the subject; biomedical engineering had yet to become fashionable. Sir Saeed recalls checking a government website and seeing that it touted biomedical engineering as the “number one topic for promoting careers in engineering”. This sort of thinking led to a flood of undergraduate degree courses in the subject, and Sir Saeed may have helped that along, having worked with universities to create some of those courses.
In biomedical engineering, it helps to have experience in the medical domain. For Sir Saeed this began after he completed his master’s and took up a job as a research assistant in Strathclyde’s Department of Bioengineering working on a PhD on the alignment of artificial legs. This was followed by a further three years as a research fellow working on motion analysis – how people walk. It was good experience of how to gain knowledge and science, and how to apply that “into a real practical proposition”.
An intelligent prosthetic
🦿 The award-winning integrated prosthetic limb with four microprocessors
When Sir Saeed Zahedi and his team of engineers at Blatchford won the 2016 MacRobert Award for the Linx artificial limb, they raised the profile of prosthetics and biomedical engineering. Linx stands apart from other prosthetic lower limbs in its complexity. It is the first, and so far only, integrated prosthetic lower limb, with four microprocessors: one for the knee, one for the ankle, one for battery management and a central computer.
The work that led to the award-winning device started in 1989 when the company created the first limb with a microprocessor controller in the knee. Through the 2000s, the company began developing innovative joints that produced smoother gait and better control, and the addition of independent movement to the heel and toe of the prosthetic limb created far more fluid movements. If the wearer is walking down a slope, for example, the system recognises the angle from the sensors around the limb.
Biomechanical analysis carried out by Blatchford showed that changes in resistance of the knee joint influenced the ankle-to-foot joint and vice versa. This led to a ‘brake’ mode being developed that not only worked to stop the knee sinking forward on a downward slope, but also acted in the ankle to reduce the amount of momentum transferred to the next step by 42%. This means amputees can put less effort into resisting gravity as they descend and gives them a sense of stability and support as they walk downhill.
In 2010, the company introduced the first hydraulic ankles; later on, these were given their own microprocessor to control the amount of energy that they could absorb and release. For an above-knee amputee wearing both an artificial knee and ankle, the limbs would contain two ‘brains’ that each independently controlled the movement of each joint. However, the Linx is the first prosthetic limb to integrate the control of the knee and ankle together and produce a far more natural movement.
By combining these technologies, Blatchford believes it has been able to reduce by half the amount of extra energy a person wearing a prosthesis needs to expend to compensate for the lost limb. For example, the first microprocessor-controlled knee reduced energy expended by the wearer by 25%. Adding a microprocessor to the ankle reduced it by a further 18%, while integrating the control of both joints with a single processor in the Linx took it down by another 8%.
Engineering in the NHS
A key aspect of this time was working with patients. After six years in academic research, he moved to the NHS where he came up against another indicator of the state of his subject. The NHS did not have biomedical engineer grades, so he was told that he was a medical physicist. His role was to develop research and to manage engineering for the NHS in Dundee.
The NHS did not have biomedical engineer grades, so he was told that he was a medical physicist
Sir Saeed’s next change highlights an important issue in how biomedical engineering fits into healthcare. At the time, Scotland brought together all the activities that required biomedical engineers, including prosthetics, artificial limbs, wheelchairs and orthotics, the latter of which involve assistive devices such as braces, footwear and other services that help people to recover from or avoid injury. “The department was effectively employing professionals in parts of the multidisciplinary team to care for a varied population of people with disabilities,” he says.
This was before competition began to influence healthcare. Suppliers tendered for contracts and carried out work commissioned by the NHS. The supplier then billed the NHS on a cost-plus basis. It may have been a simple system, but Sir Saeed admits that “it wasn’t an impetus for developing technology”.
The arrival of competition in the NHS began to change things with the medical side separating from social care, so biomedical engineers were no longer covering the whole area. This prompted Sir Saeed to think moving into the private sector, where he could indulge in some of the engineering innovation that the field needed.
He was already familiar with Blatchford, one of the UK’s leading suppliers of lower-limb prosthetics and other devices. Brian Blatchford, a design engineer and a third-generation member of the family owned business, had been a visitor to Strathclyde, and had seen the need to apply engineering to prosthetics. The artificial leg had not advanced much in thousands of years, says Sir Saeed. “The most radical change was at the turn of the 20th century,” he adds. “The US Navy was essentially doing research and providing articulated ankles, but it was still very much a wooden leg, a Long John Silver type of device.”
Changing lives
These were interesting times for Sir Saeed. In quick succession, he was due to get married and had to choose between two job offers, which also meant moving house. “At that age, you have a lot of energy, so somehow things worked out,” he explains. “I ended up moving to Blatchford as coordinator of research and development (R&D).” There he could follow up Brian Blatchford’s idea of mass producing lower-limb prosthetics, and providing extra functionality by applying engineering principles and designed articulated joints as standard items. “Modularity meant that you mass produced knees and ankles, rather than making them individually,” he adds. “Then you put them together like Meccano and make the interfaces for the individuals.”

Professor Sir Saeed Zahedi OBE RDI FREng (centre) with the Blatchford team that won the 2016 MacRobert Award
The move to Blatchford meant that Sir Saeed could get stuck into R&D for prosthetics. “At once, I saw that my role was to bring in the knowledge and science gained working in the university.” He had a staff of around 30 people, who not only worked on new prosthetics but also the next generation of mass-produced engineering. “Suddenly, you find yourself uniquely positioned,” he adds. “You have academic and clinical experience, and now you’re working in industry. In those days, in our field, having this combination of three was often unheard of.” One surprise, he recounts, is that at Blatchford “you could cut across all of the noise about profit and focus on the user.” This was an ideal environment to develop the concept of patient experience and user-centred design.
An important part of that process involved understanding how individuals walk. Simple prosthetics could not adapt to the way an amputee walked. An artificial leg swung at a constant rate, forcing the wearer to adapt how they moved, so that it was obvious when someone was wearing a false leg.
“Despite spending six years studying biomechanics and amputee locomotion and four years in the clinic, it didn’t dawn on me that, if I am going to get up from here to go to that door, I change my speed five times,” Sir Saeed explains. “We now understand a lot more about what you need, as an amputee, to get up from a chair, what you need to stand, what you need to be able to stand on a slope, come down the stairs, go up the stairs.” That knowledge all fed into Blatchford’s development programme.
Despite spending six years studying biomechanics and amputee locomotion and four years in the clinic, it didn’t dawn on me that, if I am going to get up from here to go to that door, I change my speed five times
Sir Saeed’s arrival at Blatchford also coincided with a change in the thinking about what amputees could achieve. Soon after joining the company in 1988 he went to Japan to see the first amputee running ‘leg over leg’, with both feet off the ground. “Amputees never thought that they could run,” says Sir Saeed. By 2012, hundreds of amputee runners had participated in the Paralympics, breaking records in the process.
Another change around the time that Sir Saeed went to Japan was the rising number of injured soldiers returning from the Gulf War. Much of the impetus, and the knowledge that drives innovation at Blatchford, comes from working with injured soldiers at the Defence and National Rehabilitation Centre in Nottinghamshire. These patients are especially demanding of their prosthetics. As Sir Saeed describes it, their attitude is that when they had a below-knee amputation “it was just a scratch”.
These factors helped to change the shape of prosthetics. As Sir Saeed sums up the situation: “The equipment is there, the motivation is there and the support is there, so you have these key factors. If they come together then everything is possible.”
Future of mobility
These possibilities do not stop with amputees. There is now growing interest in the broader area of mobility for people with disabilities. Sir Saeed is also involved in the World Health Organization’s (WHO) GATE initiative (Global Cooperation on Assistive Technology), a 10-year programme that includes mobility as its number one topic, encompassing prosthetics, orthotics and wheelchairs. WHO estimates that “more than two billion people will need at least one assistive product by 2030”. As Sir Saeed sees it: “literally one seventh or one eighth of the population will be disabled or aged. They need assistive technology devices, they need mobility devices to be able to go from A to B and be independent.”
One challenge that Sir Saeed highlights is the perceived high cost of mobility aids. He points out that these devices can pay for themselves. “If people are mobile they can have a more independent life. Not only can they look after themselves, they can contribute to society.”
We not only design and manufacture products, we look after one-third of the amputees in the UK
For that to happen, prices must come down. Advanced prosthetics and orthotics are not cheap. While those in medical circles may be prepared to pay £50,000 for an artificial heart, there is a reluctance to spend a lot on prosthetics and orthotics. Once again, the split between medical treatment and social services comes into play. At the moment, there are three different pots of funding for prosthetics and orthotics in the UK. NHS England looks after prosthetics, hospital commissioning groups handle orthotics and social services are in charge of wheelchairs. “In Norway, there is one combined funding pot,” which makes sense to Sir Saeed. “You need that medical care, but you also need, more importantly, social care.”
Blatchford covers all bases and ends up working with different agencies. “We not only design and manufacture products, we look after one-third of the amputees in the UK,” Sir Saeed says. “We are service providers to the NHS.” This gives Saeed an invaluable resource. “I have access to 250 clinicians, who are a part of my team. I have access to 14,000 amputees so I can get their opinions directly.”
Career timeline and distinctions
Born, 1957. Studied mechanical engineering at the Polytechnic of Central London, 1975–1978. PhD in biomedical engineering at the University of Strathclyde, 1978–1984. Awarded an OBE for services to the prosthetics industry, 2000. Joined Blatchford Group as Head of Research and Development, 2004. Appointed Technical Director at Blatchford Group, 2006. Fellow of the Royal Academy of Engineering, 2012. Appointed Royal Designer for Industry by the Royal Society of Arts, 2013. British Healthcare Trades Association Lifetime Achievement Award, 2013. Knighted for services to engineering and innovation, 2017. American Orthotic and Prosthetic Association Lifetime Achievement Award, 2017.
Engaging the public
One unexpected spinoff from Blatchford’s activities is the publicity value in prosthetics. When the company started using carbon fibre in artificial legs, the media rushed to write about it. Sir Saeed is happy to exploit this interest in the wider cause of engineering. Like many eminent engineers, he is frustrated by the perception of engineers. He recalls that, as a student, he was president of the university’s engineering society. “One of the things that was quite strange and difficult to understand was why society saw engineers as effectively advanced plumbers or electricians, whereas the lawyers and doctors were different.” Thirty years on and he believes “the same applies”.
A knock-on from this misperception is that too few students think ‘engineering’ when trying to choose what to study and a career option. It turns out that bioengineering, and working with prosthetics, can help to tear down those barriers. Sir Saeed recounts his work with the University of Southampton and school students. At the end of a day’s activities, much of it around prosthetics, he asked for a show of hands about how many would not go on into engineering. “Two showed their hands.” It turned out that those two wanted to study medicine, while the other 38 wanted to be engineers.
Sir Saeed’s desire to “catch them young” kicked in when he was part of the Blatchford team that won the MacRobert Award. “The team agreed that we wanted to use it to promote engineering, and the key thing is to excite the kids.” It turns out that one way to do this is to introduce them to sporting amputees running the 100 metres. Not only did the students pay attention, their teachers sat up and took notice. Teachers and pupils had an opportunity to see what engineering and people with disabilities could achieve together. “If you can nurture those brains you will get the next generation of biomedical engineers, who will not only solve this problem but much greater problems.”
***
This article has been adapted from "Bodies of work", which originally appeared in the print edition of Ingenia 77 (December 2018).
Contributors
Michael Kenward OBE
Author
Keep up-to-date with Ingenia for free
SubscribeRelated content
Health & medical

Kidney dialysis
Small haemodialysis machines have been developed that will allow more people to treat themselves at home. The SC+ system that has been developed is lighter, smaller and easier to use than existing machines.

Engineering polymath wins major award
The 2015 Queen Elizabeth Prize for Engineering has been awarded to the ground-breaking chemical engineer Dr Robert Langer FREng for his revolutionary advances and leadership in engineering at the interface between chemistry and medicine.
Blast mitigation and injury treatment
The Royal British Legion Centre for Blast Injury Studies is a world-renowned research facility based at Imperial College London. Its director, Professor Anthony Bull FREng, explains how a multidisciplinary team is helping protect, treat and rehabilitate people who are exposed to explosive forces.
Targeting cancers with magnetism
Cambridge-based Endomag has helped treat more than 6,000 breast cancer patients across 20 countries. The MacRobert finalist uses magnetic fields to power diagnostic and therapeutic devices. Find about the challenges that surround the development and acceptance of medical innovations.
Other content from Ingenia
Quick read

- Environment & sustainability
- Opinion
A young engineer’s perspective on the good, the bad and the ugly of COP27

- Environment & sustainability
- Issue 95
How do we pay for net zero technologies?
Quick read

- Transport
- Mechanical
- How I got here
Electrifying trains and STEMAZING outreach

- Civil & structural
- Environment & sustainability
- Issue 95