
Thermal scanner aims to reduce amputation risk for people with diabetes
Impaired wound healing is one of the major complications of diabetes. In severe cases, it can cause a kind of skin sore called an ulcer, to which feet are especially susceptible. If foot ulcers become infected, patients may require toe, foot, or leg amputations – as is the case for over 7,000 people with diabetes in the UK each year.
The levels are similar in North America and Northern Europe, and are growing. On top of the life-changing trauma for individuals, a 2020 analysis from Diabetes UK estimated that £1 of every £140 the NHS spends is on diabetic foot care.
A 2020 analysis from Diabetes UK estimated that £1 of every £140 the NHS spends is on diabetic foot care.
People with diabetes are advised to look after their feet and inspect them daily, but this isn’t always physically easy or convenient to do, for instance, for those with mobility issues. The current standard of care from the NHS is an annual foot check from a diabetic foot nurse or GP, although higher risk patients may be checked every three or four weeks.
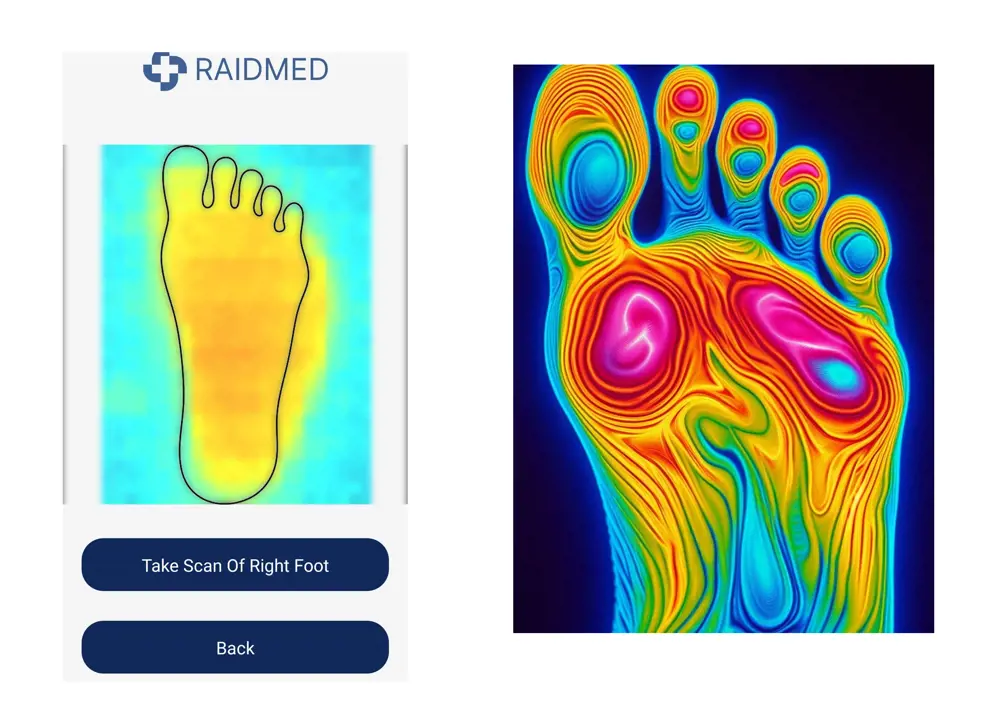
While these tests give an accurate measure of foot health on the day of the test, circumstances can change quickly. “Diabetic foot disease can very easily progress from an injury to an infection to an ulcer,” says David Branagh, founder of diabetes-focused medtech startup Raidmed. Electronics engineer David founded Raidmed in 2022, after learning of the challenges associated with diabetes footcare and the need for an urgent solution. Ever since, the company has been working on a portable, low-cost thermal imaging solution to detect foot ulcers in people with diabetes earlier, and therefore prevent lower limb amputations.
© Raidmed
Using temperature to monitor foot health
After an electrical engineering degree and several years in telecoms and audio device engineering, David’s journey to working on diabetes care was influenced by a desire to make “tech for good”. “I enjoy solving technical challenges, such as in telecommunications and consumer audio where my early career was spent, but am really drawn to challenges where the tangible impact is visible – where I can witness the direct positive result of my efforts.”
One of the first projects like this he worked on was a wireless wearable called Aingel (Gaelic for ‘angel’), used to monitor patients’ vital signs after major surgeries such as hip replacements. Such devices are increasingly important where health services are overstretched – a trend showing no sign of reversing. “It’s providing continuous monitoring at a cost and convenience that works in a hospital,” he says.
[I] am really drawn to challenges where the tangible impact is visible – where I can witness the direct positive result of my efforts
David Branagh
With Raidmed, David brought his experience in developing low-cost wireless medical devices together with a body of clinical data showing the effectiveness of monitoring foot temperature as a proxy for foot health in people with diabetes. The prime example of this data was a clinical trial in the US that sent study participants home with a contact thermometer and asked them to measure six points on both feet each day. If an area was two degrees warmer (or more) than other areas, this meant the patient was at risk of developing an ulcer and required a face-to-face consultation with their clinician to inspect their feet. But while measuring six different points on each foot with a thermometer was highly effective in a trial setting, it was also time-consuming for participants, and so not a long-term solution.
Researchers in another study tried a different tack, bringing people with diabetes into clinics once a month to take a high-resolution thermal image of their feet. Unfortunately, it was shown to have no significant benefit – reflecting, again, the potential for rapid changes in foot condition.
Making foot monitoring a daily routine
In the hopes of catching ulcers before they can form, Raidmed has developed an Internet of Things-connected thermal sensing device that enables people with diabetes and their clinicians to monitor foot health and detect potential inflammation that may develop into an ulcer.
In effect, the system has turned the approach demonstrated by the clinical trial into a user-friendly, all-in-one device, with which people at risk can conduct a simple daily test to monitor foot temperature. It can be done from home, with data passed onto clinicians remotely, or in a care setting.
Operation is simple: the patient lines up their foot with the device, which sits on the floor, to take a thermal image. A connected smartphone app shows them the image and shares test data with their clinician via the cloud, giving early warning of the signs associated with the risk of diabetic foot disease.
He hopes Raidmed’s intervention will avert up to 80% of diabetic lower limb amputations, reducing healthcare costs at the same time

© Raidmed
David explains that its AI-based data analysis “enables early detection of foot inflammation, even before the skin is broken”. He hopes Raidmed’s intervention will avert up to 80% of diabetic lower limb amputations, reducing healthcare costs at the same time.
In developing the device, the team has drawn from a wealth of feedback from people with diabetes through interviews, which confirmed foot health as a major concern. And it’s not just patients who have provided valuable insights. “Diabetes is a disease that benefits from a broad range of clinical expertise,” says David, citing podiatric surgeons working in limb preservation, vascular surgeons, nutritionists, and endocrinologists among the experts Raidmed has consulted.
In 2023, David was awarded funding and support through the Royal Academy of Engineering’s Regional Talent Engines programme. This helped the team refine its product and secure funds to further develop it. “Raising finance in medtech is a challenge and working with the Academy, we have had access to a range of financing options and secured valued funding.”
Raidmed’s prototype is now undergoing testing and validation with its intended user base, including through collaboration with NHS trusts. Through these trials, the team plans to gather additional user feedback and refine its data analysis algorithms. This will also help in obtaining regulatory approvals to bring its product to market.
For the 10% of the estimated five million people in the UK with diabetes likely to develop a foot ulcer, the roll out of David’s innovation cannot come soon enough.
Keep up-to-date with Ingenia for free
SubscribeRelated content
Health & medical

Kidney dialysis
Small haemodialysis machines have been developed that will allow more people to treat themselves at home. The SC+ system that has been developed is lighter, smaller and easier to use than existing machines.

Engineering polymath wins major award
The 2015 Queen Elizabeth Prize for Engineering has been awarded to the ground-breaking chemical engineer Dr Robert Langer FREng for his revolutionary advances and leadership in engineering at the interface between chemistry and medicine.
Blast mitigation and injury treatment
The Royal British Legion Centre for Blast Injury Studies is a world-renowned research facility based at Imperial College London. Its director, Professor Anthony Bull FREng, explains how a multidisciplinary team is helping protect, treat and rehabilitate people who are exposed to explosive forces.
Targeting cancers with magnetism
Cambridge-based Endomag has helped treat more than 6,000 breast cancer patients across 20 countries. The MacRobert finalist uses magnetic fields to power diagnostic and therapeutic devices. Find about the challenges that surround the development and acceptance of medical innovations.
Other content from Ingenia
Quick read

- Environment & sustainability
- Opinion
A young engineer’s perspective on the good, the bad and the ugly of COP27

- Environment & sustainability
- Issue 95
How do we pay for net zero technologies?
Quick read

- Transport
- Mechanical
- How I got here
Electrifying trains and STEMAZING outreach

- Civil & structural
- Environment & sustainability
- Issue 95